Poverty during Childhood and Adolescence May Predict Long-term Health
by Natalie Troxel and Paul Hastings, UC Davis
Growing up in poverty may have long-term impacts beyond the chance of a better financial future. The stress of early-life poverty may in fact be associated with serious health problems well into adulthood.
Ongoing research by Center Graduate Student Fellow Natalie Troxel and Faculty Affiliate Paul Hastings examines the association between poverty and compromised adult health, which may have implications for healthcare costs in the U.S.
Key Findings
- High blood pressure, elevated glucose levels and being overweight are associated with each other and can be combined into a single index of risk for health problems.
- Among individuals in this study, neighborhood affluence, neighborhood safety, and family resources during childhood and adolescence together accounted for 4.5% of the differences between their health risk indexes 15 to 20 years later.
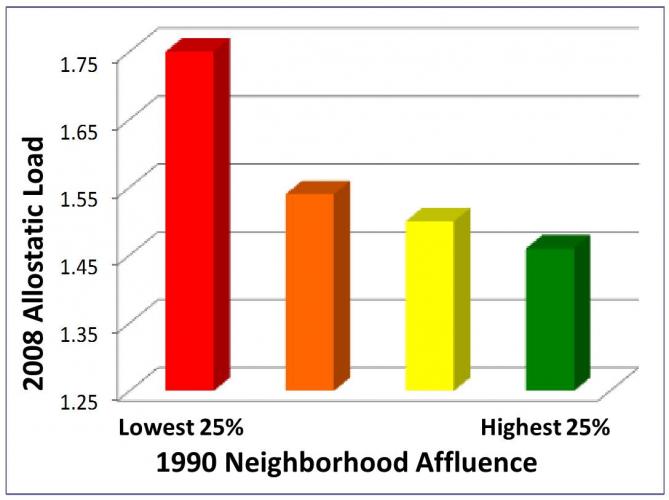
- Having a lower level of neighborhood affluence in childhood or adolescence was the single strongest predictor of biological risk for health problems in adulthood.
More than one in five U.S. children come from families whose incomes fall below the 2010 federal poverty level of $22,314 per year for a family of four. Research has shown that being raised in an impoverished environment can have lasting effects on children’s physical and mental well-being. With U.S. healthcare expenditures of nearly 18 percent of GDP in 2010, and treatment of chronic diseases such as asthma, diabetes, and heart disease accounting for over 75 percent of all national health expenditures, it is important to consider the possible long-term health impacts of growing up in poverty.
The human body is constantly adapting to environmental stresses, like being exposed to flu viruses at work or being caught in rush-hour traffic. The body copes with these stresses by adjusting the activity of immune, neurological, metabolic, and other biological systems. Constant adjustments, however, can have a negative impact on long-term health.
“Allostatic load” is a measure of the wear and tear on the body caused by this constant adaptation to stress. It indicates the point at which the body can no longer adapt. In other words, the strain of prolonged exposure to stress—such as living in poverty—can over-tax the body’s self-regulatory abilities and lock the body into an unhealthy state. This could leave children and youth vulnerable to many chronic health problems such as cardiovascular disease, diabetes and depression, which may persist into adulthood.
Add Health Data
Researchers used data from the National Longitudinal Study of
Adolescent Health (Add Health) to investigate the relationship
between childhood poverty and allostatic load in young adulthood.
Add Health followed a nationally representative cohort of
adolescents who were in grades 7-12 during the 1994-95 school
year, and consists of four waves of data collection. The analyses
reported below used a subset of the total sample (N = 1,449; 46
percent female).
This study included Add Health Wave 1 data, collected when participants were 11-21 years old, and Wave 4 data, collected in 2008 when the participants were between 24 and 33 years old. Measures of allostatic load came from the Wave 4 Add Health data and included participants’ blood glucose levels, body mass, blood pressure, presence of C-reactive protein (an indicator of inflammation) and glycated hemoglobin (an indicator of diabetes).
The study included three measures of socioeconomic indicators: family resources, neighborhood safety, and neighborhood affluence. The first two were measured in Add Health Wave 1 data. Neighborhood affluence was obtained from 1990 census data and was linked to each participant by block group census areas.
The Health Impact of Poverty
After controlling for gender (significantly associated with
allostatic load), family resources, neighborhood safety, and
neighborhood affluence all significantly and independently
predicted adult allostatic load. Individuals raised in poverty
showed more indicators of health problems approximately 15 to 20
years later, depending on the measure of socioeconomic
indicators. Among the adults in this study, the three economic
measures together accounted for 4.5 percent of differences in
their respective health risk indices.
Although 4.5 percent appears modest, it can have larger implications from a public health perspective when extended out to the hundreds of millions of people in the U.S. The association between poverty and allostatic load falls between the magnitude of the link between a daily aspirin and reduced heart attack risk, and smoking tobacco and increased risk of lung cancer.
Of the three significant socioeconomic predictors of allostatic load, neighborhood-level affluence was the strongest predictor. Youths raised in neighborhoods with lower median incomes and higher unemployment and poverty rates showed higher degrees of allostatic load in adulthood. The factors of family resources and neighborhood safety were roughly equivalent to one another in their predictive power.
The fact that the strongest association was between neighborhood affluence and allostatic load may be because of the robust and objective nature of census data, or because these data were collected four years earlier than data on family resources and neighborhood safety measures. Therefore the measure of neighborhood characteristics from the 1990 census reflected economic factors during the participants’ childhood to late-adolescent period of physical development. This could suggest that the chronic stress of poverty when experienced earlier in life may be even more strongly associated with compromised adult health.
Health Policy for the Long-term
The overall results of these analyses indicate that poverty
experienced during childhood and adolescence has a significant,
though moderate, association with indicators of compromised
physical health in adulthood. Given the long-term national and
individual costs of treating chronic illnesses, it is likely that
many of these adults may remain economically distressed
throughout their lives as chronic health problems occur, thus
creating a feedback cycle which increases the probability that
their own children will suffer health consequences associated
with being raised in circumstances of economic distress.
From a policy perspective, these analyses suggest that it may be more effective and economical to interrupt this cycle by focusing interventions on neighborhoods at risk, rather than focusing on specific at-risk youth or families.
Meet the Researchers
Natalie Troxel is a Ph.D. candidate in Psychology at UC
Davis. Her research interests include families-at-risk and
long-term effects of childhood poverty.
Paul Hastings is Chair and Professor of Psychology at UC Davis. His research centers around understanding the ways in which biological and environmental factors shape the trajectories of children’s emotional and social development.