Rises in Chronic Illness Greatest Among Disadvantaged Youth
By Lauren Wisk, UCLA, and Niraj Sharma, Brigham and Women’s Hospital
In a recent study, we investigated pediatric-onset conditions in the US, seeking to identify recent trends as well as opportunities for prevention and intervention. Specifically, we analyzed chronic conditions (CC) and functional limitations (FLs) in more than 236,000 children (5-17 years) and young adults (18-25 years) between 1999 and 2018.
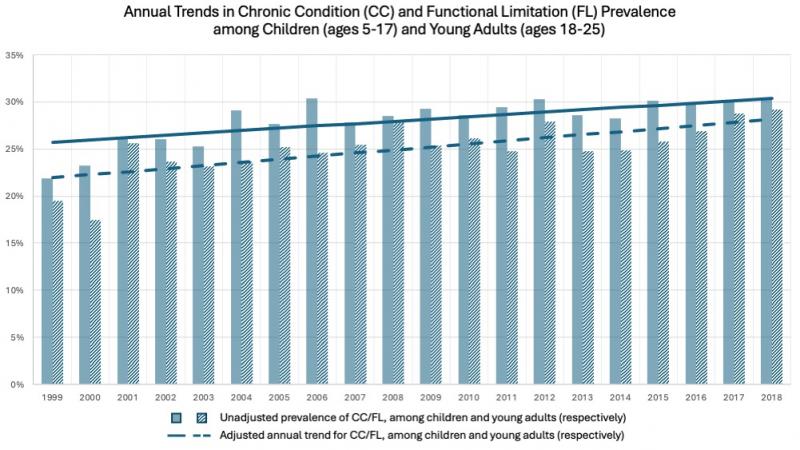
We found that the prevalence of children with a CC/FL rose from 22.57 percent in 1999/2000 to 30.21 percent in 2017/8 – an adjusted annual increase of 0.24 percentage points, or about 130,000 additional children, per year. Among young adults, the prevalence increased from 18.49 percent to 29.01 percent over the same period, for an annual rise of 0.33 percentage points or an additional 80,000 young adults each year. For both age groups, the leading contributors to this increase were asthma and mental/behavioral health conditions. We also found evidence of growing socioeconomic disparities in the prevalence of many conditions.
Policymakers seeking to reduce these disparities and improve the health of America’s young people should implement policies that support disadvantaged children and young adults, improving their access to health insurance, medical care, and food and housing security
Key Facts
- The prevalence of US youth living with a chronic condition or functional limitation has risen over the past two decades from around 1-in-5 youth to nearly 1-in-3 youth, amounting to over 25 million children and young adults.
- Socioeconomic disparities in prevalence mean that individuals with chronic illness are more likely to be (or have parents/carers who are) poor, unemployed, and have public insurance.
- Policymakers seeking to reduce these disparities and improve the health of America’s young people should implement policies that improve their access to health insurance, medical care, and food and housing security.
Background
Studies suggest that between 12 and 30 percent of youth and young adults in the US suffer from CCs and/or FLs, and that this prevalence is growing.[1] Changes to social conditions (such as increased income inequality) and more recently the COVID-19 pandemic (with its connection to worsening mental health) may contribute to expanded prevalence in years to come.[2,3,4]
There is also evidence for growing disparities.5 Youth with CCs and FLs are subject to high healthcare-related financial burden, poor quality of life, poor educational attainment, and low social and community participation.[6,7,8,9] As such, growing disparities in the prevalence of these conditions have the potential to impact future adult social and economic disparities. This in turn would likely have major implications for public and private health expenditures, workforce participation, and quality-adjusted life years. Understanding the scope of this problem is a critical first step for designing supportive programs and policies that can mitigate the negative effects of growing up with a chronic illness.
In our study[10], we sought to provide an update on the prevalence of youth and young adults in the US who are currently living with a CC or FL (and thus need access to medical care and/or supportive services) while also assessing for socioeconomic differences in prevalence. We also wished to determine how the prevalence of such conditions has changed over the past two decades (prior to the COVID-19 pandemic), and estimate the number of youth who enter adulthood with a CC or FL each year.
Examining the prevalence of chronic conditions and functional limitations
We obtained 20 years of National Health Interview Survey (NHIS) data, collected between 1999 and 2018. NHIS collects health information annually for a nationally representative, cross-sectional sample of the civilian, noninstitutionalized population in the US. We identified CCs if individuals reported having ever or recently been diagnosed with a condition that is typically pediatric-onset and expected to be persistent or severe. Examples of these conditions include asthma, cystic fibrosis, and diabetes. We identified FLs similarly, with respondents answering a series of questions to determine if they had any limitations, and then being asked to specify the underlying condition causing said limitations from a pre-specified list of conditions. We also compiled sociodemographic data, including respondents’ age, sex, race/ethnicity, total combined income of all family members as a percentage of the federal poverty level, and employment status (for young adults, their own; for children, their parent’s/parents’).
We first analyzed data descriptively before going on to employ multivariate linear probability models to estimate annual average increase in prevalence of CC/FL and differences in average CC/FL prevalence across sociodemographic predictors. We also used regression models adjusted for sociodemographic characteristics to estimate the adjusted annual trend in prevalence accounting for demographic changes over time.
Clear socioeconomic disparities in rising prevalence of CC and FL
Across all years, 28.1 percent of children had a reported CC/FL, with an unadjusted annual increase in prevalence of 0.32 percentage points (pp) per year. After adjustment for sociodemographic characteristics, the annual increase in prevalence was 0.24 pp per year. We identified numerous socioeconomic disparities. Youth living below the federal poverty level had 3.39 pp higher adjusted prevalence than the highest income families. Compared to privately insured youth, those with public insurance or combination public and private had 8.63 pp and 21.54 pp higher prevalence respectively. Those with partial coverage had 5.75 pp higher prevalence while uninsured youth had 2.17 pp lower prevalence. Regarding employment, prevalence was 7.65 pp higher for children with unemployed parents compared to those who parents were employed.
Among young adults, across all years, 25.1 percent reported a CC/FL, with an unadjusted annual increase in prevalence of 0.35 pp per year. After adjustment for sociodemographic characteristics, the annual increase in prevalence was 0.33 pp per year. As with children, socioeconomic disparities were evident. Young adults those living below the federal poverty level had 3.11 pp higher adjusted prevalence than those with the highest income. Compared to privately insured young adults, those with public insurance or combination public and private had 10.58 pp and 27.24 pp higher prevalence respectively. Those with partial coverage had 6.09 pp higher prevalence. The unemployed had 3.93 pp higher prevalence than the employed. Adjusted prevalence decreased with increasing levels of education.
Increasing prevalence of CC was primarily driven by ADHD/ADD, autism, and asthma for children, and by asthma, seizures/epilepsy, and prediabetes for young adults. Increasing prevalence in FL was primarily driven by speech conditions, ‘other’ mental health conditions (e.g., ADHD/ADD), and depression/anxiety/emotional problems for children, and by musculoskeletal problems, depression/anxiety/emotional problems, and ‘other’ mental health conditions for young adults.
Break the cycle of socioeconomic disadvantage and chronic illness with targeted health and social policies
The prevalence of US youth living with a chronic condition or functional limitation has risen over the past two decades from around 1-in-5 youth to nearly 1-in-3 youth, amounting to over 25 million US youth ages 5-25 at present population levels. This increase highlights the critical importance of public health and primary prevention efforts in the pediatric care setting to reduce current burden on youth and the future burden on the adult health system. New policy incentives are clearly needed to ensure that youth are able to maintain continuous access to care and other supportive services as they age. Policymakers will want to consider a range of responses that address different sectors such as school/employment, housing/independent living, and frequently transition in community/social spheres.
We found that individuals with chronic illness were more likely to be poor, unemployed, and have public insurance. Given the lower socioeconomic status that many of these individuals face, policy decisions must be implemented to ensure that this growing population continues to be supported in the future. These can include continued and expanded funding for Medicaid to support this population. The level of poverty and parental unemployment further suggests the importance of ongoing social services for these individuals, such as those that target income, food, and housing insecurity. As an example, improving educational and employment opportunities can ensure better access to health insurance and medical care while improving food and housing insecurity can ameliorate chronic conditions such as asthma.
Our findings suggest that a vicious cycle may exist for pediatric-onset conditions whereby socioeconomic disadvantage is perpetuated throughout the life-course. Breaking this cycle will rely on targeted health and social policies that both ameliorate family disadvantage during childhood and ensure equal opportunity for social, educational, and vocational participation for youth as they age into adulthood.
Lauren Wisk is an assistant professor in the Division of General Internal Medicine & Health Services Research at UCLA.
Niraj Sharma is a program director at Brigham and Women’s Hospital and an assistant professor of internal medicine and pediatrics at Harvard Medical School.
References
1. Delaney L, Smith JP. Childhood health: trends and consequences over the life course. Future Child. 2012;22(1):43-63. doi:10.1353/foc.2012.0003
2. Emerson E. Relative child poverty, income inequality, wealth, and health. JAMA. 2009;301(4):425-426. doi:10.1001/jama.2009.8
3. Meherali S, Punjani N, Louie-Poon S, et al. Mental Health of Children and Adolescents Amidst COVID-19 and Past Pandemics: A Rapid Systematic Review. Int J Environ Res Public Health. 2021;18(7):3432. doi:10.3390/ijerph18073432
4. Lebrun-Harris LA, Ghandour RM, Kogan MD, Warren MD. Five-Year Trends in US Children’s Health and Well-being, 2016-2020. JAMA Pediatr. 2022;176(7):e220056. doi:10.1001/jamapediatrics.2022.0056
5. Newacheck PW, Stein RE, Bauman L, Hung YY; Research Consortium on Children with Chronic Conditions. Disparities in the prevalence of disability between black and white children. Arch Pediatr Adolesc Med. 2003;157(3):244-248. doi:10.1001/archpedi.157.3.244
6. Wisk LE, Peltz A, Galbraith AA. Changes in Health Care-Related Financial Burden for US Families with Children Associated with the Affordable Care Act. JAMA Pediatr. 2020;174(11):1032-1040. doi:10.1001/jamapediatrics.2020.3973
7. Silva N, Pereira M, Otto C, Ravens-Sieberer U, Canavarro MC, Bullinger M. Do 8- to 18-year-old children/adolescents with chronic physical health conditions have worse health-related quality of life than their healthy peers? A meta-analysis of studies using the KIDSCREEN questionnaires. Qual Life Res. 2019;28(7):1725-1750. doi:10.1007/s11136-019-02189-7
8. Wisk LE, Weitzman ER. Expectancy and Achievement Gaps in Educational Attainment and Subsequent Adverse Health Effects Among Adolescents with and Without Chronic Medical Conditions. J Adolesc Health. 2017;61(4):461-470. doi:10.1016/j.jadohealth.2017.04.006
9. Noonan K, Reichman NE, Corman H, Jiménez ME. School and Community Involvement of Adolescents with Chronic Health Conditions. J Adolesc Health. 2020;67(4):576-582. doi:10.1016/j.jadohealth.2020.02.028
10. Wisk, LE, Sharma, N. Prevalence and Trends in Pediatric-Onset Chronic Conditions in the United States, 1999-2018. Academic Pediatrics. 2025. doi:10.1016/j.acap.2025.102810









