Reduce Inequality to Bolster Societal Resilience: Lessons From the COVID-19 Pandemic
By Anna M. Parenteau, Chase J. Boyer, Lillian J. Campos, Angelica F. Carranza, LillyBelle K. Deer, Ph.D., Dana T. Hartman, Julie T. Bidwell, Ph.D., R.N. and Camelia E. Hostinar, Ph.D., University of California, Davis
Social and economic inequality are chronic stressors that continually erode the mental and physical health of marginalized groups, undermining overall societal resilience. In a recent review, we synthesized evidence of greater increases in mental health symptoms during the COVID-19 pandemic among socially or economically marginalized groups in the United States, including people who are low-income or experiencing homelessness.[1] Based on our findings, we propose that reducing social and economic inequality would promote population mental health and societal resilience to future crises. Specifically, we propose interventions to bolster societal resilience by enhancing economic safety and equity.
Key Facts
- The increase in the prevalence and severity of mental health problems during the COVID-19 pandemic was stratified based on socioeconomic status.
- Those problems increased and intensified most dramatically among people who were low-income or experiencing homelessness.
- Reducing social and economic inequality would promote population mental health and societal resilience to future crises.
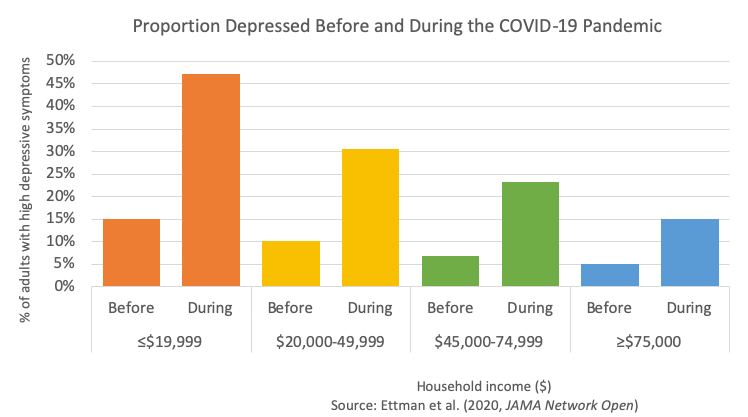
The COVID-19 pandemic brought about an overall increase in the prevalence of mental health problems. These problems were, however, stratified based on socioeconomic status (SES). For example, higher levels of depression symptoms affected those who had lower income, less than $5,000 in savings, and who experienced more stressors.[2] A different study found that participants whose income fell below the federal poverty level had 4.58 times higher odds of developing significant distress during the pandemic compared to those above the poverty level.[3] Another noted that food insufficiency was associated with worse mental health during the pandemic, particularly symptoms of anxiety and depression.[4]
COVID-19 visited particular vulnerability upon people experiencing homelessness or unstable housing. This group suffered higher rates of infection and illness than the general population, and exhibited high rates of comorbidity with psychiatric illness and substance use.[5] Particularly affected were adolescent and young-adult substance users who were homeless, with one study estimating that 16%-28% reported increased use of alcohol, tobacco, and marijuana after the onset of the pandemic.[6] With shelter in place mandates and economic instability limiting residential mobility during the pandemic’s first year, incidences of intimate partner violence increased, and victims were placed at a greater risk for experiencing homelessness.[7]
Explaining COVID’s disproportionate effects
Although the COVID-19 pandemic is unique in the severity of its health, social, and economic disruptions, its disproportionate impact on lower-SES groups was largely predictable on three bases. Firstly, high SES provided greater protection against wage losses and more opportunities for remote work, as well as greater flexibility to avoid public transportation and crowding.[8] In turn, this flexibility protected higher SES people against escalating mental health problems.
Secondly, social and economic inequality function as chronic stressors that activate stress-response systems, eroding the mental and physical health of socially and economically marginalized groups. These groups can be expected to experience exacerbated neurobiological stress responses during new crises like the pandemic.
Thirdly, for low-income groups, mental-health deterioration and higher rates of COVID-19 morbidity and mortality were inextricably linked to pre-existing chronic diseases known to be more prevalent among socially and economically marginalized groups, such as cardiovascular, metabolic, and immune conditions. Thus, as the pandemic has shown, social inequality can create a worsening spiral of mutually reinforcing mental and physical health problems.
Bolstering economic safety and equity
With the brunt of the COVID-19 pandemic having been experienced by lower-resourced communities, economic safety and equity should be prime targets for promoting population mental health and societal resilience. To promote such resilience to future calamities, existing economic “safety net” policies require expansion, and new policies need consideration and examination. These include cash transfer and income supplement programs, broader food assistance programs, and more support for housing and residential mobility.
Sustained cash transfer programs piloted in other nations have been shown to reduce stress, prevent family violence, and increase long-term living standards.[9] A monthly child allowance has been projected to completely eliminate severe child poverty in the United States, potentially disrupting intergenerational cycles of poverty.[10] The Child Tax Credit is an example of a policy that has been effective at reducing the rate of child and family poverty to historic lows.[11] Cash transfers and child allowances have also shown more efficacy in reducing food insecurity in Canada than the Supplemental Nutrition Assistance Program (SNAP) in the United States, a program tied to income and limited in eligibility terms.
Additionally, housing unaffordability remains a structural barrier to disaster resilience. Providing permanent housing to the unhoused has become urgent during the COVID-19 pandemic and has increased popularity for innovative policies that successfully address housing insecurity. For people living in high-poverty neighborhoods, residential mobility programs such as Moving to Opportunity have shown reductions in personal distress and improved wellbeing 15 years later. Among individuals from high-poverty neighborhoods, one standard deviation reduction in neighborhood poverty reduced stress to levels equivalent to those of individuals above the poverty line.[12] Community investments and residential mobility opportunities can be offered in tandem to improve communities for those who wish to remain and provide flexibility for individuals and families seeking new communities. These poverty reduction measures may promote resiliency among higher-level systems, allowing lower-level systems to adapt to stress.
Expand the safety net to increase resilience
Individuals who are marginalized along multiple dimensions of their identity (e.g., being a low-income woman, or an LGBTQ adolescent with a prior history of multiple childhood adversities) have experienced a more negative impact of the pandemic on their mental health. This is because multiple forms of inequality interact and intersect to shape an individual’s experience and health in unique ways according to their social identity.
For instance, women with lower socioeconomic status and marginalized racial or ethnic identities experienced greater disadvantage during the COVID-19 pandemic and were overburdened in ways that impacted their well-being and mental health.[13] The compounding effects of these multiple identities suggest the need to allocate additional resources and interventions for those who experience multiple forms of social or economic disadvantage. Expanding economic “safety net” policies that promote economic safety and equity will create greater resilience among communities and families before a disaster occurs, allowing a more robust and adaptive response.
Camelia Hostinar is an associate professor of psychology at UC Davis.
Anna Parenteau, Chase Boyer, Lillian Campos, Angelica Carranza, and Dana Hartman are PhD students at UC Davis.
LillyBelle Deer is a postdoctoral scholar at the University of Denver.
Julie Bidwell is an assistant professor of nursing at UC Davis.
References
1. Parenteau, A. M., Boyer, C. J., Campos, L. J., Carranza, A. F., Deer, L. K., Hartman, D. T., Bidwell, J.T., & Hostinar, C. E. (2022). A review of mental health disparities during COVID-19: Evidence, mechanisms, and policy recommendations for promoting societal resilience. Development and Psychopathology, 1-22, https://doi.org/10.1017/S0954579422000499
2. Ettman, C. K., Abdalla, S. M., Cohen, G. H., Sampson, L., Vivier, P. M., & Galea, S. (2020). Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Network Open, 3(9), e2019686. doi: 10.1001/jamanetworkopen.2020.19686.
3. Riehm, K. E., Holingue, C., Smail, E. J., Kapteyn, A., Bennett, D., Thrul, J., Kreuter, F., McGinty, E. E., Kalb, L. G., Veldhuis, C. B., Johnson, R. M., Fallin, M. D., & Stuart, E. A. (2021). Trajectories of Mental Distress Among U.S. Adults During the COVID-19 Pandemic. Annals of Behavioral Medicine, 55(2), 93 102. https://doi.org/10.1093/abm/kaaa126
4. Nagata, J. M., Ganson, K. T., Whittle, H. J., Chu, J., Harris, O. O., Tsai, A. C., & Weiser, S. D. (2021). Food insufficiency and mental health in the U.S. during the COVID-19 pandemic. American Journal of Preventative Medicine, S0749-3797(21)00012-X. doi: 10.1016/j.amepre.2020.12.004. Epub ahead of print.
5. Fuchs, J. D., Carter, H. C., Evans, J., Graham-Squire, D., Imbert, E., Bloome, J., & Kanzaria, H. K. (2021). Assessment of a hotel-based COVID-19 isolation and quarantine strategy for persons experiencing homelessness. JAMA Network Open, 4(3), e210490. doi: 10.1001/jamanetworkopen.2021.0490.
6. Tucker, J. S., D’Amico, E. J., Pedersen, E. R., Garvey, R., Rodriguez, A., & Klein, D. J. (2020). Behavioral health and service usage during the COVID-19 pandemic among emerging adults currently or recently experiencing homelessness. Journal of Adolescent Health, 67(4), 603-605. doi: 10.1016/j.jadohealth.2020.07.013.
7. Goodsmith, N., Ijadi-Maghsoodi, R., Melendez, R. M., & Dossett E. C. (2021). Addressing the urgent housing needs of vulnerable women in the era of COVID-19: The Los Angeles county experience. Psychiatric Services, 72(3), 349-352. doi: 10.1176/appi.ps.202000318.
8. Brough, R., Freedman, M., & Phillips, D. C. (2021). Understanding socioeconomic disparities in travel behavior during the COVID-19 pandemic. Journal of Regional Science, 10.1111/jors.12527. Advance online publication. https://doi.org/10.1111/jors.12527
9. Haushofer, J., Ringdal, C., Shapiro, J. P., & Wang, X. Y., (2019). Income changes and intimate partner violence: Evidence from unconditional cash transfers in Kenya [Working paper]. National Bureau of Economic Research. https://www.nber.org/papers/w25627
10. Shaefer, H. L., Collyer, S., Duncan, G., Edin, K., Garfinkel, I., Harris, D., … & Yoshikawa, H. (2018). A universal child allowance: A plan to reduce poverty and income instability among children in the United States. The Russell Sage Foundation Journal of the Social Sciences, 4(2), 22–42. https://doi.org/10.7758/RSF.2018.4.2.02
11. Wise, P. H., & Chamberlain, L. J. (2022). Adversity and Opportunity: The pandemic’s paradoxical effect on child health and well-being. JAMA Pediatrics. doi:10.1001/jamapediatrics.2022.0063
12. Leventhal, T., & Brooks-Gunn, J. (2003). Moving to opportunity: An experimental study of neighborhood effects on mental health. American Journal of Public Health, 93(9), 1576–1582. https://doi.org/10.2105/ajph.93.9.1576
13. Laster Pirtle, W. N., & Wright, T. (2021). Structural Gendered Racism Revealed in Pandemic Times: Intersectional Approaches to Understanding Race and Gender Health Inequities in COVID-19. Gender & Society, 35(2), 168–179. https://doi.org/10.1177/08912432211001302










