Racial Disparities in Education Deepened by Changes to Medicaid Delivery
By Briana Ballis, University of California, Merced
Though racial disparities in infant health conditions have persisted for decades, evidence regarding their long-term consequences has been limited. In a recent study, I used administrative data from Texas and the shift to Medicaid Managed Care (MMC) to examine the later effects of prenatal MMC on key schooling outcomes.
I found that MMC-driven declines in infant health worsened cognitive and noncognitive outcomes for Black children, while MMC-driven enhancements in infant health improved noncognitive outcomes and educational attainment for Hispanics. Black children prenatally exposed to MMC saw the largest test score declines in districts that are less effective at improving outcomes for Black students, highlighting the role of targeted resources in mitigating the effects of poor infant health. In contrast, Hispanic students showed test score gains in low-value-added districts for Hispanic students, suggesting that better health can help offset the disadvantages of attending a less effective school.
Policymakers seeking to reduce racial disparities in education should take note of the long-term impacts of infant health conditions and their treatment, and consider their implications for the design of programs like MMC.
Key Facts
- In 1993, Texas transitioned to Medicaid Managed Care (MMC), with negative consequences for Black children from low-income households.
- Over time, prenatal MMC exposure significantly reduced test scores for low-income Black students.
- Policymakers seeking to reduce racial gaps in education should take note of the long-term impacts of infant health conditions and their treatment.
Background
The link between improved early life conditions and upward mobility is well established.[1] Early life interventions that increase access to health care, nutrition, and education are seen as a promising way to reduce gaps during adulthood, and indeed, extensive US public expenditures currently support vulnerable youth before the age of five.[2,3] However, despite spending on such programs amounting to about $200 billion annually, significant inequalities throughout the lifecycle persist across high- and low-income children, especially among children born into low-income Black families.[4] Black infants experience markedly worse early life health outcomes, with an infant mortality rate nearly three times higher than that of infants from all other racial groups.
The introduction of MMC in Texas in 1993 provides an ideal opportunity to investigate how declines in Black infant health influence later outcomes. MMC places more emphasis on primary care and encourages coordination among providers. It also introduces incentives to reduce healthcare utilization, employing either cost targets or capitation payments (i.e., a fixed payment per enrollee per year) to managed care organizations (MCOs) who coordinate and deliver care. The shift from traditional Medicaid fee-for-service (FFS) to MMC led to one of the most substantial shifts in racial infant health gaps a recent cohort of children to date. After the MMC transition, health gaps between Black and Hispanic infants increased by 69 percent, with Black infant health worsening and Hispanic infant health slightly improving.[5]
In my study,[6] I used the shift to MMC in Texas to explore not only the downstream consequences arising from a decline in initial health conditions.
Examining the impact of MMC on educational outcomes
I used administrative data for all children conceived in Texas between 1993 and 2001 and educated in Texas public schools. Specifically, I linked records from the Texas Birth Index with data from the Texas Schools Project covering standardized exam scores, attendance, disciplinary incidences, and special education participation. I also observed high-school completion, college enrollment and college completion. Taken together, these merged data made it possible to trace out the impacts of prenatal MMC exposure on a rich set of childhood and early adult outcomes. After applying various restrictions, I was left with 2,222,896 observations.
To establish the first-stage impact of MMC on infant health, I relied on previous research documenting significant changes in infant health disparities.[5] To identify the longer-run impact of prenatal MMC exposure on subsequent academic achievement and educational attainment, I estimated a difference-in-difference model that leveraged the county-by-county rollout of MMC between 1993 and 2001.
MMC linked to reduced test scores for low-income Black students
Over time, prenatal MMC exposure significantly reduced test scores for low-income Black students. Across grades 3 through 8, reading and math test scores declined by about 3 percent of a standard deviation (see Figure 1). During high school, I found that absences, grade repetition, and suspensions increased, suggesting declines in noncognitive skills. Given the Black-White test score gap is about 0.5 of a standard deviation, this suggests that MMC increased achievement gaps by roughly 6 percent. Black children prenatally exposed to MMC were slightly more likely to be placed in special education (roughly a 1 percentage-point increase or a 7-percent change relative to the mean of 12 percent).
In contrast, prenatal MMC exposure did not affect the short-run cognitive development of Hispanic students overall, but it improved their longer-run educational attainment and noncognitive skills throughout their entire primary and secondary schooling. This suggests that the improved infant health among Hispanics improved skills that cannot be captured by test scores but are nonetheless important for long-run success.
Looking at the overall impact masks important differences across districts with different effectiveness for Black and Hispanic children. For instance, Black children prenatally exposed to MMC experience the largest test score declines in districts that have low value-added for Black children. In contrast, while prenatal MMC exposure did not impact Hispanic test scores overall, there are positive test score gains in school districts with low value added for Hispanic children. This suggests that targeted school resources can help mitigate the effects of poor infant health on cognitive development or, conversely, mute any positive gains that improved infant health may generate.
I also examine the broader peer effects of MMC exposure within classrooms. Specifically, a 5-percent increase in Black Medicaid eligible peers corresponds to a test score decline of approximately 0.3-3.8 percent of a standard deviation.
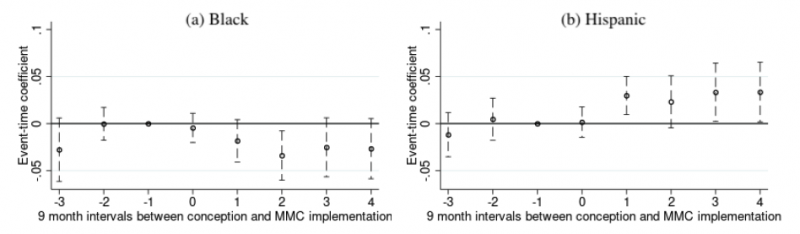
Figure 1. The impact of MMC at birth on reading test scores.
Adapt Medicaid delivery to reduce racial disparities
When it was adopted in Texas in 1993, MMC introduced significant cost-containment measures that led most healthcare providers to transition from receiving payments for individual services to capitation payments, or fixed payments per enrollee per year. This change widened infant health gaps in Texas, worsening Black children’s infant health and slightly improving Hispanic children’s infant health.
My results reveal that MMC also had meaningful effects on non-health related outcomes. Specifically, I find that prenatal MMC exposure significantly reduced test scores for low-income Black children, with reading and math test scores declining by about 3 percent of a standard deviation across grades 3 through 8. Given the Black-White test score gap is 0.5 of a standard deviation, this implies a 6-percent increase in achievement gaps. While test scores for Hispanic children were unaffected, prenatal MMC exposure improved their noncognitive outcomes and educational attainment, reinforcing the idea that test scores may not fully capture the benefits of early-life health interventions. However, in districts where schools provided lower value-added for Hispanic students, test scores did improve, suggesting that better health can help mitigate the disadvantages of attending less effective schools for one’s demographic. My analysis suggests that changes in prenatal health are the key mechanism behind these findings.
Schools in Texas remain segregated based on race, and the negative impacts of poor infant health multiply when children are exposed to peers facing similar disadvantages. My study suggests that MMC in its current form exacerbates those disadvantages. My findings can help improve cost-benefit calculations critical for effective MMC program design—particularly in relation to how the design and delivery of Medicaid may impact racial disparities throughout life.
Briana Ballis is an assistant professor of economics at UC Merced.
References
1. García, J. L., Heckman, J. J., Leaf, D. E., & Prados, M. J. (2020). Quantifying the life-cycle benefits of an influential early-childhood program. Journal of Political Economy, 128(7), 2502-2541.
2. Almond, D., Currie, J., & Duque, V. (2018, December). Childhood circumstances and adult outcomes: Act ii. Journal of Economic Literature, 56(4), 1360-1446.
3. Bailey, M. J., Hoynes, H. W., Rossin-Slater, M., & Walker, R. (2020, April). Is the social safety net a long-term investment? Large-scale evidence from the food stamps program (Working Paper No. 26942). National Bureau of Economic Research.
4. Hoynes, H. W., & Schanzenbach, D. W. (2018). Safety net investments in children. Brookings Papers on Economic Activity, 2018(1), 89-150.
5. Kuziemko, I., Meckel, K., & Rossin-Slater, M. (2018, August). Does managed care widen infant health disparities? Evidence from Texas Medicaid. American Economic Journal: Economic Policy, 10(3), 255-83.
6. Ballis, B. (2024) Early Life Health Conditions and Racial Gaps in Education. Human Capital and Economic Opportunity Working Group Working Paper.










