Poverty Associated with Stress Among California Adolescents of Mexican Origin
By Lisa E. Johnson, UC Davis; Luis A. Parra, Washington University in Saint Louis; Elisa Ugarte, UC Davis; David G. Weissman, Harvard University; Sasha G. Han, St. Bonaventure University; and Richard W. Robins, Amanda E. Guyer, Paul D. Hastings, UC Davis
Poverty is a chronic stressor, associated with disruptions in adolescent development. To illuminate those disruptions, we examined associations of chronic poverty and income changes experienced from pre- to mid-adolescence with hypothalamic-pituitary-adrenal (HPA) axis stress responses in late adolescence.
The 229 study participants were adolescents of Mexican origin. We assessed their household income annually between the ages of 10 and 16. When they were 17, we asked them to complete a social exclusion simulation task while undergoing an MRI scan, after which we collected their saliva to test levels of cortisol, a stress hormone released by the HPA axis.
We found that experiences of poverty between the ages of 10 and 16 predicted HPA axis activity at age 17. Relative to others in this sample, youth who started adolescence in deep poverty, and who were still living in poverty at age 16 despite experiencing some income gains, demonstrated distinct cortisol suppression. Youth from more economically secure families showed typical cortisol increases. These results indicate that subsequent stress responses vary as a function of economic status throughout adolescence. Furthermore, this suggests that efforts to increase family income may promote healthy HPA functioning, and consequently stress regulation, for youths in the most impoverished circumstances.
Key Facts
- Persistent poverty can jeopardize adolescent well-being, with fluctuations in family income also affecting development, particularly in low-income environments.
- In our study of 229 Mexican-origin teens, participants who experienced poverty throughout their adolescence displayed atypically low stress responses.
- Public policy programs that help alleviate poverty may improve psychological and physical health among adolescents.
Background
Chronic exposure to stressors like poverty is linked with children’s adrenocortical functioning.[1] Adolescence in particular is a developmentally-sensitive period when chronic poverty may have heightened effects.[2] Persistent poverty can jeopardize adolescent well-being to a greater extent than temporary poverty, with fluctuations in family income also affecting development, particularly in low-income environments.[3]
Relative to other sociodemographic groups, racial/ethnic minority families experience greater exposure to community crime, crowding, and systematic discrimination, all of which are associated with poverty.[4] People at the intersections of marginalized social group memberships are often disadvantaged and may experience disruptions to their adrenocortical (i.e., HPA) functioning.[5] In California, Latinx youth and families are structurally and systematically marginalized and over-represented in poverty contexts that can disrupt normative and healthy physiological activity.[6,7] In our study, we examined effects of the timing and chronicity of poverty across adolescence on HPA activity among Mexican-origin adolescents.[8]
Examining How Poverty Predicts Stress Levels
We studied 229 Mexican-origin adolescents who, along with their parents, were enrolled in a neurobiological sub-study of the California Families Project (CFP). We calculated income-to-needs ratios by dividing the family’s reported annual income from ages 10 to 16 by the income value corresponding with the poverty line for a family of that size, as indicated by the U.S. Census Bureau. Income-to-needs ratios ranged from 0 to 5, with ratios of 1 or less indicating poverty. When the participants reached the age of 17, they completed three tasks while undergoing an MRI scan. The second task was Cyberball, a virtual ball-toss game designed to elicit feelings of ostracism, social exclusion, and rejection. We collected saliva and passive drool samples before the adolescents played Cyberball, and five further times afterwards, at ten-minute intervals. We then tested these samples for cortisol before analyzing the results.
Greatest Exposure to Poverty Associated with Most Distinct Stress-Response Profiles
The mean income-to-needs at age 10 was 120 percent of the federal poverty line, with 47.8 percent of the sample living at or below the federal poverty line. At the mean level, participants did not show evidence of acute HPA reactivity to the MRI scanner and Cyberball activities. The most distinct HPA response profiles were exhibited by youths who entered adolescence living in deep poverty and, despite experiencing some income gains over the years, were still living below the poverty line at age 16. These youths evidenced a pattern of sharp cortisol decline across the initial samples, followed by slight increases in the final two samples (40–50 minutes post-Cyberball).
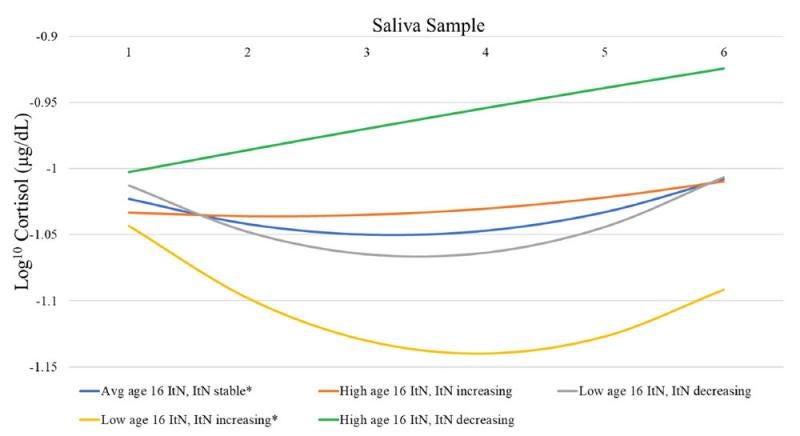
Figure 1. Youths’ HPA responses varied according to their prior socioeconomic context
Adolescents from families with lower income-to-needs at age 16, with a history of annual increases in income-to-needs from age 10 to age 16—that is, deeper poverty in early adolescence, but still impoverished at age 16—produced a cortisol profile characterized by a pronounced decrease in circulating levels across the first 4 samples, followed by a clear increase in the 5th and 6th samples (Fig. 1; yellow line). In contrast, adolescents from families whose income-to-needs remained stable across the years and reported average income-to-needs at age 16 displayed a cortisol profile characterized by slow and small decreases in cortisol across the first 4 samples, followed by a slight increase in the 5th and 6th samples (Fig. 1; blue line). Finally, adolescents from families with higher income-to-needs at age 16 with histories of increasing or decreasing income-to-needs had relatively unchanging or increasing cortisol levels, respectively, across the samples (Fig. 1; orange and green lines).
Efforts to Alleviate Poverty May Improve Teens’ Physical and Mental Health
Youths from families in deep poverty at the beginning of adolescence and, despite some income gains, remaining impoverished across the adolescent years displayed sharp and steady cortisol decreases across the saliva samples, indicative of greater HPA suppression relative to the other youths in this sample. These findings suggest that living in poverty during adolescence, particularly early adolescence, may potentially lead to blunted HPA responses. Meanwhile, for youths from economically-secure families, income losses appeared to impact adrenocortical responsiveness. For these adolescents, their family’s financial security may suddenly seem perilous, leading to increased psychological distress which may exaggerate physiological stress reactivity.
If left unregulated, HPA suppression may have serious implications for mental health, particularly for adolescents at risk for depression. Our study highlights early adolescence as a period when interventions may confer additional benefits. It captures the intersection at which two marginalized social statuses (living in low socioeconomic-status contexts and being Latinx) interact and impact adrenocortical functioning, thus contributing to a more nuanced perspective on poverty, ethnicity, and the development of adrenocortical responses.
Mexican-origin adolescents who were living in deep poverty at age 10, and who—despite experiencing some income gains—were still living below the poverty line at age 16, evinced reduced or blunted HPA activity following acute social stress. Conversely, adolescents from more economically secure families displayed increases in cortisol considered more typical.
Our findings underscore that the consequences of poverty exposure for subsequent stress physiological sensitivity continue to unfold across adolescence, a time when young people experience significant neurobiological changes and increased risk for psychopathology. As such, this study suggests that efforts to increase family income during adolescence may promote better physical and mental health for youths living in impoverished circumstances.
Lisa E. Johnson is a PhD candidate at UC Davis. Luis A. Parra is a research assistant professor at Washington University in Saint Louis. Elisa Ugarte is a PhD candidate at UC Davis. David G. Weissman is a postdoctoral fellow at Harvard University. Sasha G. Han is a visiting assistant professor of psychology at St. Bonaventure University. Richard W. Robins is a professor of psychology at UC Davis. Amanda E. Guyer is a professor of human ecology at UC Davis. Paul D. Hastings is a professor of psychology at UC Davis.
References
[1] Evans, G.W., Chen, E., Miller, G., Seeman, T., 2012. How poverty gets under the skin: a life course perspective. The Oxford Handbook of Poverty and Child Development. Oxford University Press.
[2] Mazza, J.R.S., Lambert, J., Zunzunegui, M.V., Tremblay, R.E., Boivin, M., Cote, S.M., 2017. Early adolescence behavior problems and timing of poverty during childhood: a comparison of lifecourse models. Soc. Sci. Med. 177, 35–42.
[3.] Duncan, G.J., Magnuson, K., Votruba-Drzal, E., 2014. Boosting family income to promote child development. Future Child. 99–120.
[4.] Roy, A.L., Raver, C.C., 2014. Are all risks equal? Early experiences of poverty-related risk and children’s functioning. J. Fam. Psychol. 28 (3), 391.
[5.] Parra, L.A., Hastings, P.D., 2018. Integrating the neurobiology of minority stress with an intersectionality framework for LGBTQ-Latinx populations. New Dir. Child Adolesc. Dev. (161), 91–108.
[6.] Annie E. Casey Foundation, 2017. Race for results: building a path to opportunity for all children. AECF. www.aecf.org.
[7.] Myers, H.F., 2009. Ethnicity-and socio-economic status-related stresses in context: an integrative review and conceptual model. J. Behav. Med. 32 (1), 9–19.
[8.] Johnson, L.E., Parra, L.A, Ugarte, E., Weissman, D.G., Han, S.G., Robins, R.W., Guyer, A.E., Hastings, P.D., 2021. Patterns of poverty across adolescence predict salivary cortisol stress responses in Mexican-origin youths. Psychoneuroendocrinology. 132. 105340. https://doi.org/10.1016/j.psyneuen.2021.105340










