Nutrition-Program Revisions Associated with Improved Maternal and Infant Health
By Rita Hamad, Daniel F. Collin, and Laura L. Jelliffe-Pawlowski (UC San Francisco), and Rebecca J. Baer (UC San Diego)
The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) serves more than one-quarter of pregnant and postpartum women in the United States. In October 2009, the WIC food package underwent revisions to improve nutritional content. In a recent quasi-experimental study of more than two million California infants, we investigated the extent to which those revisions—which increased access to whole grains, fruits, vegetables, and low-fat milk—resulted in improvements in maternal and infant health. We found the revised WIC food package to be associated with reduced maternal preeclampsia and gestational weight gain, as well as improved infant gestational age and healthier birth weights. Our findings suggest that improving pregnant women’s nutrition may be an important target of clinical interventions and health policy.
Key Facts
The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) serves more than one-quarter of pregnant and postpartum women in the US.
In October 2009, the WIC food package was revised to improve nutrition and reduce obesity and chronic disease.
The revised WIC package is associated with improvements in maternal and infant health.
Maternal nutrition is an important determinant of fetal development.[1] Evidence points to the long-term effects of fetal programming—the environment surrounding the fetus as it develops in utero—on children’s health.[2] This is likely due to changes in fetal hormones, metabolism, and other physiologic processes. The transmission of disadvantage during pregnancy may explain the intergenerational persistence of health disparities in the United States.[3]
Intended to reduce such disparities, WIC is a federal program for low-income pregnant and postpartum women and children younger than five years. It provides nutritional support, nutrition education, breastfeeding support, and referrals to health and social services to more than a quarter of pregnant and postpartum women in the US.[4] The program has a proven track record of success. For example, its introduction in the mid-1970s resulted in higher birth weights, particularly for less-educated mothers. Similar findings have emerged in more recent years.[5]
In October 2009, after criticism that the standard WIC food package had been essentially unchanged for more than 30 years, the US Department of Agriculture implemented major revisions to the program.[6] The revised food package, which included more whole grains, fruits, vegetables, and low-fat milk, was intended to be more nutritious, thereby addressing obesity and chronic disease. This revised package increased household expenditures on whole grains and decreased purchasing of refined grains and whole milk among WIC recipients.[7] It also led to improvements in maternal and child nutrition.
In our study, using data from more than two million births in California, we examined whether the revised WIC food package also affected perinatal health.[8] Specifically, we compared pre-post policy changes among WIC recipients with pre-post changes in a control group of nonrecipients. This enabled us to estimate the associations of program revisions with outcomes such as birth weight.
Analyzing Outcomes Before and After the Revised WIC Package
We used data from January 2007 to December 2012 from the California Office of State Health Planning and Development database. This database contains linked birth certificates and hospital discharge records for mothers and infants from one year before birth to one year after birth. We included California singleton infants live-born from 2007 to 2012 with a gestational age of 20 to 44 weeks at delivery. The final sample included 2,897,537 infants born to 2,441,658 mothers.
In designing our analysis, we selected maternal and infant outcomes that could be affected by the mother’s receipt of the revised food package. Maternal outcomes included whether the mother was diagnosed as having preeclampsia or gestational diabetes. We also calculated whether the mother gained less weight, more weight, or was within recommended gestational weight gain (GWG) according to guidelines from the Institute of Medicine (now the National Academy of Medicine). To account for sociodemographic variables, we adjusted models for mother’s education, age, race/ethnicity, and parity and infant’s sex and year of birth.
Once analysis began, we first tabulated sample characteristics among WIC recipients and non-recipients who gave birth before and after implementation of the revised food package. We then estimated the associations of the revised food package with outcomes using difference-in-difference analysis. Given that the WIC package was revised in October 2009, we noted that a mother who gave birth in February 2010 or later was exposed to the revised food package for at least half of her pregnancy, while a mother who gave birth before February 2010 was exposed to the revised package for less than half of her pregnancy or not at all. We thus compared WIC recipients who gave birth on or after February 2010 with those who gave birth before February 2010.
Revised Package Benefits Mothers and Infants
For mothers, we found that the revised food package was associated with reduced likelihood of both preeclampsia (−0.6 percentage points) and more-than-recommended GWG (−3.2 percentage points). We also found it to be associated with an increased likelihood of both less-than-recommended GWG (0.9 percentage points) and within-recommended GWG (2.3 percentage points).
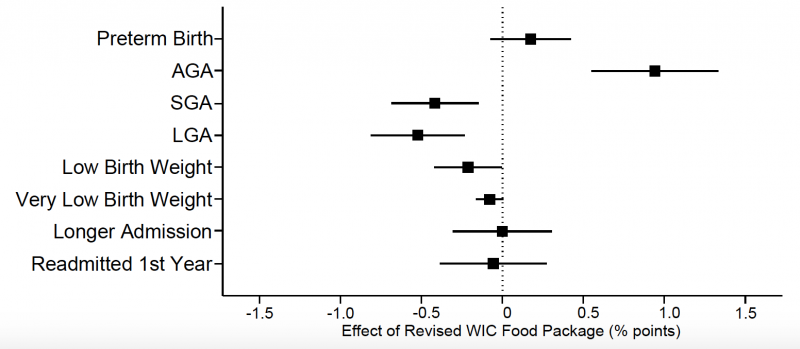
Infants of WIC recipients exposed to the revised food package had a mean gestational age at birth that was longer by 0.2 weeks. In terms of birth weight based on gestational age, they were more likely to have an appropriate weight (0.9 percentage points) and less likely to be small (−0.4 percentage points) or large (−0.5 percentage points). They were also less likely to have low birth weight overall (−0.2 percentage points). In the figure below, which charts these infant outcomes, AGA stands for appropriate for gestational age, with SGA and LGA standing for small and large respectively.
Improving Perinatal Nutrition Can Reduce Health Disparities
The revised WIC food package was intended to improve maternal nutrition by providing more whole grains, fruits, vegetables, and low-fat milk. We found improvements in perinatal health, including maternal preeclampsia and weight gain, gestational age, and appropriate birth weight for gestational age. In several cases, the magnitude of the findings represents a clinically meaningful change, which is likely to have a substantial impact at the population level. For example, the reduction in preeclampsia of 0.6 percentage points represents a 17 percent reduction from a base of 3.5 percent. For infant-health outcomes, effect sizes were more modest perhaps because these represent outcomes further downstream from the primary intervention. Nevertheless, these findings suggest improved maternal nutrition translated into improvements in newborn outcomes.
Overall, revisions to improve the nutritional content of the WIC food package in October 2009 were associated with improvements in maternal and infant health at the population level, with inconsistent differences by race/ethnicity. Given that WIC is among the largest safety net programs for vulnerable families in the US, with more than a quarter of pregnant and postpartum women receiving it, our findings should be incorporated into future cost-benefit analyses of the program. They suggest that social policy may be an important lever to reduce health disparities, and strengthen the evidence for improving maternal nutrition during pregnancy.
Rita Hamad is an Assistant Professor of Family & Community Medicine at UC San Francisco.
Daniel F. Collin is a Research Analyst at UC San Francisco.
Rebecca J. Baer is a Senior Statistician at UC San Diego.
Laura L. Jelliffe-Pawlowski is an Associate Professor of Epidemiology at UC San Francisco.
This policy brief was supported by funding from the UC Office of the President Multicampus Research Programs and Initiatives, Grant MRI-19-601054.
Funding for the work on which this brief is based was provided by the National Institutes of Health (grant K08-HL132106), the University of California San Francisco National Center of Excellence in Women’s Health, and the California Preterm Birth Initiative at the University of California San Francisco.
References
[1] Barker DJP. Maternal nutrition, fetal nutrition, and disease in later life. Nutrition. 1997;13(9):807-813. doi:10.1016/S0899-9007(97)00193-7
[2] Wu G, Bazer FW, Cudd TA, Meininger CJ, Spencer TE. Maternal nutrition and fetal development. J Nutr. 2004;134(9):2169-2172. doi:10.1093/jn/134.9.2169
[3] Aizer A, Currie J. The intergenerational transmission of inequality: maternal disadvantage and health at birth. Science. 2014;344(6186):856-861. doi:10.1126/science.1251872
[4] Bitler MP, Currie J, Scholz JK. WIC eligibility and participation. J Hum Resour. 2003;38:1139-1179. doi:10.2307/3558984
[5] Bitler MP, Currie J. Does WIC work? the effects of WIC on pregnancy and birth outcomes. J Policy Anal Manage. 2005;24(1):73-91. doi:10.1002/pam.20070
[6] Institute of Medicine. WIC Food Packages: Time for a Change. Washington, DC: National Academies Press; 2006.
[7] Oh M, Jensen HH, Rahkovsky I. Did revisions to the WIC program affect household expenditures on whole grains? Appl Econ Perspect Policy. 2016; 38 (4):578-598. doi:10.1093/aepp/ppw020
[8] Hamad R, Collin DF, Baer RJ, Jelliffe-Pawlowski LL. Association of Revised WIC Food Package With Perinatal and Birth Outcomes: A Quasi-Experimental Study . JAMA Pediatr. Published online July 01, 2019. 173(9):845–852. doi:10.1001/jamapediatrics.2019.170698









