Growing Up in Poverty Increases Risk of Developing Psychosis-spectrum Disorders in Adulthood
By Paul D. Hastings, University of California, Davis; Lisa A. Serbin, William Bukowski, Dale M. Stack, Daniel J. Dickson, and Alex E. Schwartzman, Concordia University; Jonathan L. Helm, San Diego State University; Jane E. Ledingham, University of Ottawa
A person’s risk for developing psychosis-spectrum disorders such as schizophrenia in adulthood is determined by multiple factors. With this in mind, we examined the risk for the development of such disorders in a two-generation, 30-year prospective longitudinal study of 3,905 urban families in Montréal, Canada. This study took place against a sociocultural backdrop of changing economic and social conditions. We found that individuals who were both highly aggressive and highly withdrawn were at greater risk for other psychosis-spectrum diagnoses when they experienced greater neighborhood disadvantage in childhood or worsening neighborhood conditions as they aged. Childhood neighborhood disadvantage predicted both schizophrenia and bipolar diagnoses, regardless of childhood social behavior. Our results suggest that policy interventions aimed at improving neighborhood conditions may help to decrease the prevalence of psychosis-spectrum diagnoses in the future.
Key Facts
- Environmental contexts contribute to individuals’ risk for developing psychosis-spectrum disorders in adulthood.
- Children growing up in impoverished urban neighborhoods are more likely to receive consistent diagnoses of schizophrenia and bipolar disorder as they age.
- Policy interventions to address the needs of families living in poverty may help to reduce the future prevalence of costly psychiatric diagnoses.
The factors affecting mental health are both biological and environmental.[1] Parents’ own psychosis-spectrum diagnoses predict increased risk for such diagnoses in their offspring.[2] There is also now considerable evidence pointing to links between childhood poverty and growing up in disadvantaged neighborhoods and adult psychosis-spectrum disorders.[3,4] A critical question addressed in our recent study is whether childhood socioeconomic conditions predict adult psychosis-spectrum diagnoses over and above the risk associated with parents’ diagnoses. If such a link between childhood conditions and adult diagnoses exists, purely hereditary explanations would seem to be inadequate.
There are many potential reasons that childhood family or neighborhood poverty could affect future mental health above and beyond parental mental health diagnoses.[5] These include exposure to more environmental toxins, more crime, lower quality schools, fewer community resources, and increased parental distress, among others.[6] Prior studies have shown that the risks for mental-health problems, including psychosis-spectrum diagnoses, increase in accordance with the duration of children’s and adolescents’ exposure to neighborhood impoverishment.[7] Our study shows that such increased risk remains even after accounting for psychosis-spectrum disorders among children’s parents.
Measuring Psychiatric Status and Socioecological Circumstances
Using data from the Concordia Longitudinal Research Project—initiated in the inner-city neighborhoods of Montréal, Québec, in 1976—we conducted an intergenerational, longitudinal study of nearly 4,000 families monitored over 30 years. The subjects of the study included two generations of each family, the parents and the children. Members of the parent generation in the Concordia Project were primarily born between the 1930s and 1950s and their children (who were the focal targets of this study) were born between 1965 and 1971.
Combining records for these two generations with numerically coded health records provided by Québec’s health ministry, we assigned five mutually exclusive categories of adult psychiatric status to members of both generations. These were Schizophrenia; Bipolar diagnosis with psychosis; Other psychosis-spectrum diagnosis (i.e., schizoaffective disorder); Non-psychotic diagnoses (e.g., depression); and No diagnosis. We also used census tract data from 1986 and 2006 to assess neighborhood socioeconomic disadvantage based on income, education, employment, and father presence. Finally, we measured social-emotional characteristics in childhood for the children using peer reports of aggression, social withdrawal, and likeability provided by 4,100 of their classmates.
With these data, we were able to examine the extent to which adult psychiatric diagnoses were associated with childhood experiences of neighborhood socioecological disadvantage, as well as stability of (or change in) neighborhood disadvantage from childhood to adulthood in a large sample of individuals for whom social behavior was assessed in middle childhood to preadolescence. Importantly, we were able to discern the effect of neighborhood disadvantage over and above any hereditary link between mental health diagnosis of parents and their children.
Impoverished Neighborhoods Contribute to Development of Psychoses
Our investigation revealed three specific factors that contributed to the probability of being diagnosed with psychosis-spectrum disorders in adulthood, even after accounting for parents’ own diagnoses. These were social behaviors with peers in childhood, neighborhood-level socioecological conditions in childhood, and changing socioecological contexts over maturation. Children in the 1970s who were raised in the most socioeconomically disadvantaged neighborhoods were at the greatest risk of being consistently diagnosed with either schizophrenia or bipolar disorder with psychosis by the time they were in middle adulthood. Further, those individuals who were diagnosed with either schizophrenia or bipolar disorder with psychosis also were likely to experience a worsening of neighborhood socioeconomic conditions as they matured from childhood into adulthood (see Figure 1).
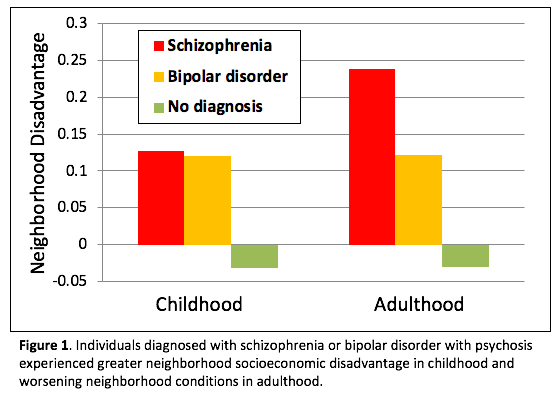
In addition, diagnoses of other psychosis-spectrum disorders were associated with both disadvantaged neighborhoods in childhood and worsening neighborhood conditions from childhood to adulthood, though these were moderated by childhood social behaviors. Specifically, those children who were seen by their peers at school as being both highly aggressive and highly socially withdrawn were more likely to be diagnosed with other psychosis-spectrum disorders, but only if they had been raised in more disadvantaged neighborhoods or if they experienced worsening neighborhood conditions as they became adults.
At 6.25 percent of the sample, the prevalence of all psychoses diagnoses not attributable to physical ailments was higher than most other estimates of psychoses by mid-adulthood.[8] This may be attributable to the targeted recruitment of an urban, predominantly lower-income sample.
Policy Interventions May Reduce Prevalence of Costly Psychiatric Diagnoses
Our study found clear evidence that children’s environmental contexts contribute to their risk for manifesting psychosis-spectrum disorders such as schizophrenia in adulthood. Beyond the risk entailed by parental diagnoses, being raised in socioeconomically disadvantaged neighborhoods contributed to the emergence of all psychosis-spectrum disorders. This was particularly true for children who had been seen as highly aggressive and withdrawn by their peers
These results suggest that economic and social policy interventions to address the needs of all families living in impoverished neighborhoods may prove effective for reducing the future prevalence of debilitating and costly psychiatric diagnoses. While this study does not identify the specific factors within disadvantaged neighborhoods that drive this association, working with socioeconomically disadvantaged neighborhoods to take steps such as improving school quality, providing safe parks and community facilities, reducing pollution, and creating local employment opportunities have potential to reduce the prevalence of future psychosis-spectrum mental illnesses. This potential to reduce rates of mental illness should be considered along with better known effects of such efforts, such as reducing future respiratory, cardiovascular and other physical illnesses, and increasing the likelihood of successful school completion and gainful employment.
Paul D. Hastings is Professor of Psychology at the University of California, Davis. Lisa A. Serbin is Professor of Psychology at Concordia University. William Bukowski is Professor of Psychology at Concordia University. Jonathan L. Helm is Assistant Professor of Psychology at San Diego State University. Dale M. Stack is Professor of Psychology at Concordia University. Daniel J. Dickson is a Postdoctoral Fellow in Psychology at Concordia University. Jane E. Ledingham is a Professor Emeritus of Psychology at the University of Ottawa. Alex E. Schwartzman was a Distinguished Professor Emeritus of Psychology at Concordia University.
References
[1] Bronfenbrenner, U., & Ceci, S. J. (1994). Nature-nurture reconceptualized in developmental perspective: A bioecological model. Psychological Review, 101(4), 568–586. doi: 10.1037/0033-295X.101.4.568
[2] Rasic, D., Hajek, T., Alda, M., & Uher, R. (2014). Risk of mental illness in offspring of parents with schizophrenia, bipolar disorder, and major depressive disorder: A meta-analysis of family high-risk studies. Schizophrenia Bulletin, 40, 28–38. doi: 10.1093/schbul/sbt114
[3] Kwok, W. (2014). Is there evidence that social class at birth increases risk of psychosis? A systematic review. International Journal of Social Psychiatry, 60, 801–808.
[4] O’Donoghue, B., Roche, E., & Lane, A. (2016). Neighbourhood-level social deprivation and the risk of psychotic disorders: A systematic review. Social Psychiatry and Psychiatric Epidemiology, 51, 941–950.
[5] McEwen, B. S., & Stellar, E. (1993). Stress and the individual: Mechanisms leading to disease. Archives of Internal Medicine, 153, 2093–2101. doi: 10.1001/archinte.1993.00410180039004
[6] Page, M. E., Conger, K., Guyer, A. E, Hastings, P. D., & Thompson, R. (2016). Children and the intergenerational transmission of poverty: Research frontiers and policy implications. Center for Poverty Research, University of California Davis.
[7] Leventhal, T., & Dupéré, V. (2011). Moving to opportunity: Does long-term exposure to ‘low-poverty’ neighborhoods make a difference for adolescents? Social Science and Medicine, 73, 737–743.
[8] Perälä, J., Suvisaari, J., Saarni, S. I., Kuoppasalmi, K., Isometsä, E., et al. (2007). Lifetime prevalence of psychotic and bipolar I disorders in a general population. Archives of General Psychiatry, 64, 19-28.










